Health equity, health disparities, and health inequities have become familiar terms in healthcare, but their intertwinement often causes confusion.
Since the announcement of the Accountable Care Organization (ACO) Realizing Equity, Access, and Community Health (REACH), there has been an inundation of conversations around health equity. But what does it really mean and how will ACO REACH help everyone achieve their highest level of health?
The Centers for Medicare & Medicaid Services (CMS) defines health equity as:
“The attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.”
How can we achieve health equity? We can do this by working collaboratively with all healthcare stakeholders to address social determinants of health (SDOH) and health disparities.
Health equity, health disparities, and health inequities have become familiar terms in healthcare, but their intertwinement often causes confusion. In their work to advance health equity, the Centers for Disease Control and Prevention (CDC) has defined the following:
| Health Equity | Health Disparities | Health Inequities |
|---|---|---|
| State in which everyone has a fair and just opportunity to attain their highest level of health | Preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that have been disadvantaged by their social or economic status, geographic location, and environment | Disparities in health that stem from unjust, systemic policies and practices which limit opportunities for good health. |
Health Inequities
Health inequities occur when health outcomes differ across groups due to systematic, avoidable, and unjust social and economic policies and practices that create barriers to opportunity. These inequities have a significant social and economic impact on individuals and societies.
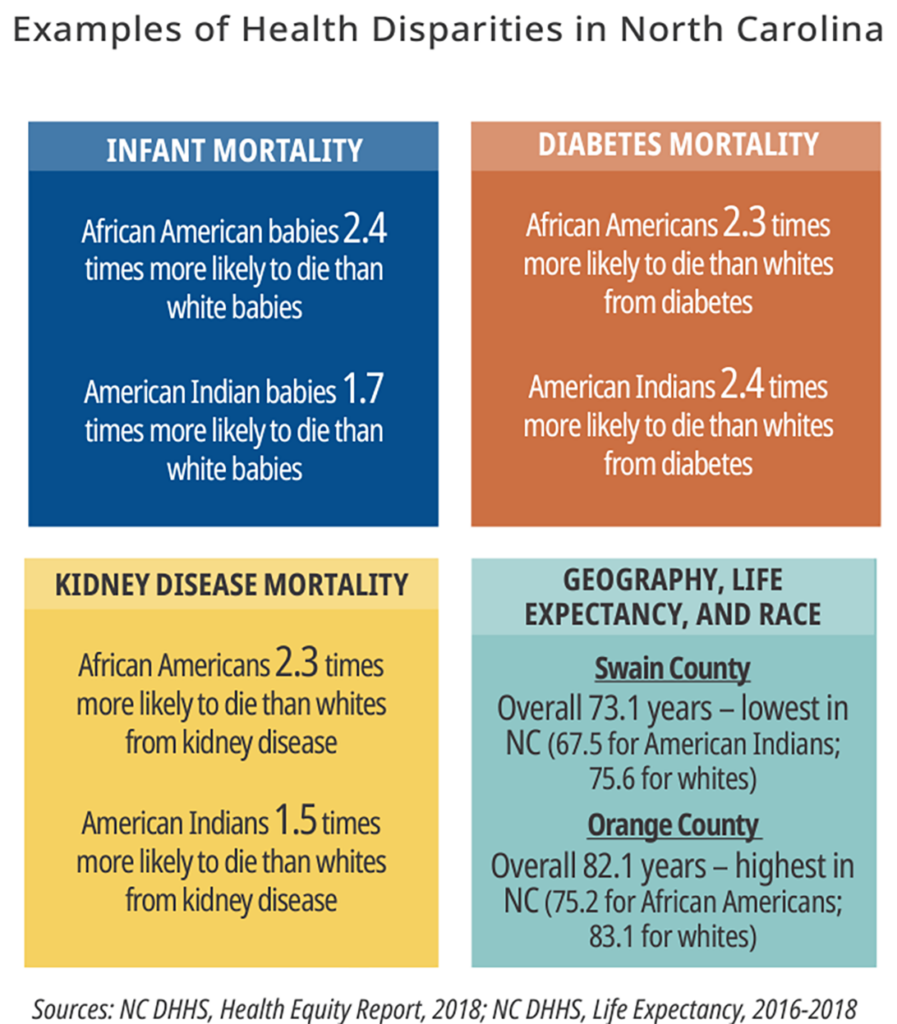
An example of a health inequity in the U.S. is the issue of race and diabetes management. Studies consistently show that racial inequities are causing health disparities in Black, American Indian, and Alaskan Natives, with the rate of diabetes as high as 14.5% for American Indians compared to a rate of 7.4% for non-Hispanic whites.
Health Disparity
A health disparity is an unavoidable and unfair difference that affects an individual’s ability to reach their optimal health. Examples include race, gender, education, income, disability, geographic location, and sexual orientation. A health disparity is often beyond an individual’s control and caused by health inequities.
Health disparities are the metric used to measure progress toward achieving health equity.
Health Equity
Health equity is the attainment of the highest level of health for all people. To achieve health equity, obstacles to positive outcomes must be eliminated. These obstacles include poverty, discrimination, and their consequences, including lack of access to goods, quality education and housing, and safe environments.
The Center for Medicare & Medicaid Innovation (The Innovation Center) believes that equitable care is necessary to achieve high-quality care for Medicare beneficiaries. As such, the Innovation Center has introduced ACO REACH, which will test a payment approach to better support care delivery and coordination for patients in underserved communities.
The ACO REACH Model is introducing five new policies to promote Health Equity starting in PY2023 (https://innovation.cms.gov/media/document/aco-reach-health-equity-slides)
- Health Equity Plan
- Health Equity Benchmark Adjustment
- Health Equity Data Collection Requirement
- Nurse Practitioner Services Benefit Enhancement
- Health Equity Questions in Application and Scoring for Health Equity
Accomplishing health equity will take time and significant effort to address. With the help of the new ACO REACH model, CHESS is excited to continue the journey towards better health for all people.
The statements contained in this document are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this document.
View All Resources